In the movie The Nutty Professor starring Eddie Murphy, the obese character Cletus sits at the dinner table, pouring tons of rich gravy onto his plate. His son, Sherman, tries unsuccessfully to warn him about the risks of eating unhealthy foods.
Cletus responds in ebonics: “Where all the calories is? You know where that come from? Watching that damn TV. Every time you turn it on, somebody talkin’ about lose weight, get healthy. Everybody lookin’ all anorexic, talkin’ about that’s healthy. I know what healthy is.”
Though Cletus is fictional, his attitude is one that rings true in the black community. Black people are more likely to suffer from hypertension (high blood pressure), heart disease and other cardiovascular disorders than other segments of the United States population.
February is American Heart Month, and the American Heart Association is encouraging people of all ethnic backgrounds to get “heart healthy.” The message should particularly resonate with the African Diaspora, which is disproportionately afflicted.
According to the AHA’s website, high blood pressure killed 56,561 people in the United States in 2006. For every 100,000 deaths, 51.1 percent were black males, and 37.7 percent were black females.
Black males were 30 percent more likely to die from heart disease, and nearly 49 percent of black women were found to have some form of heart disease, stroke or other cardiovascular disease.
Add to this the results from another AHA study which found that heart disease is a leading cause of death among women. But fewer than half of black women are aware of this fact, according to AHA.
Half the women surveyed said they would not call 911 while experiencing heart attack symptoms, but would rather opt to medically unproven treatments to deal with the pain.
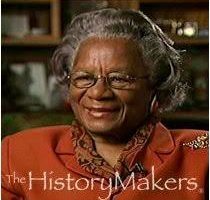
Eddye Rogers, a 68-year-old African-American woman with a family history of cardiovascular disease, used to be in that number.
“I had poor eating habits and I was overweight with high blood pressure and high cholesterol. At first, I thought it was just gas when I felt this Z-shaped pain across my back, so I continued to do what I was doing,” said Rogers, who had surgery in late 2009 to prevent a dissected aortic aneurysm from rupturing in her body.
Usually the result of high blood pressure, which causes the walls of the artery to deteriorate and eventually tear, an aortic aneurysm is often a fatal disorder.
Although she went to the Cleveland Clinic in Weston and sat in the parking lot, Rogers said she returned home to see if the pain would subside. When it didn’t let up after several hours, she went back to the emergency room.
“I went to the store and got some GAS-X, and then waited around for a while. At about 4 or 5 in the morning, the pain was just sitting on my chest, so I told my husband to take me back to Cleveland Clinic,” Rogers said
When the doctors took note of Rogers’ condition, they immediately rushed her into surgery.
“I asked them if there was another alternative and they responded, ‘No,’” Rogers said.
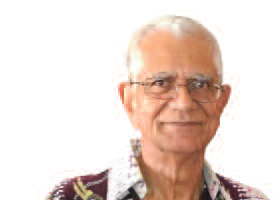
Rogers made a full recovery after being placed under the care of Dr. Edward Savage, a top-rated cardiothoracic surgeon with over 15 years of experience in treating patients with cardiovascular disorders.
“If I had to rate Dr. Savage and his staff, I would put him in a class above excellence. While I was in the hospital, everything was superior across the board,” Rogers said.
Though Savage heralds Rogers’ case as a success story, he cautioned that when it comes to hypertension and heart disease, deaths can be high in any group if the problems are not properly treated.
“I don’t see this as a race issue as much as I see it as a sex issue,” Savage joked. “Women tend to get more check-ups than men, yet African Americans in general are more prone to cardiovascular diseases.”
He continued: “Go and have a regular check-up. When we’re kids, we get check-ups periodically, and when we grow up, lots of times we get away from that. Just because you feel good doesn’t mean you don’t have high blood pressure.”
Rogers is taking his advice.
“I have a diet of low salt; I eat plenty of vegetables and I don’t fry food anymore,’’ she said. “I also exercise and go to my follow-ups because Dr. Savage and his staff told me what steps to take and now it’s on me.”
EmyprealCommunications@Gmail.com
For more information on how to be “heart healthy,” visit the American Heart Association online at www.americanheart.org.










No Comment